In males, high testosterone levels can cause changes in their mood, increased growth of body hair, high sex drive, and more.
Testosterone is a male sex hormone. It shapes many aspects of a man’s health, from mood and energy to muscles and libido. But when a man’s testosterone levels increase from the normal range, it can have noticeable effects. In this post, we’ll discuss the signs of high testosterone in men, exploring both physical changes and internal effects.
Why You Should Care
Most people think that high testosterone in men is automatically a good thing. After all, higher testosterone levels are linked to men’s strength, confidence, and drive. But in reality, it is not like that.
Just like any other biological system, balance is important. Low amounts of testosterone can drain your energy and mood, but too high amounts can bring unwanted side effects. That’s why recognizing the signs of high testosterone levels is important for you. They let you know that something in your hormone balance may need attention.
Physical Signs of High Testosterone in a Man
Men with high testosterone often see the following physical signs:
Rapid Muscle Gains & Lean Body Composition
One of the most obvious physical signs of high testosterone in a man is sudden muscle growth. The T hormone fuels protein synthesis and muscle repair, which results in rapid muscle growth.
Look at yourself in the mirror. Are your clothes fitting differently? A sudden increase in your lean muscles and a drop in fat without any changes in diet or exercise also indicates an increase in testosterone. It might seem like a benefit to you, but it is worth noting.
Unlike normal bulking, this muscle increase happens quickly. At the same time, body fat usually drops. So, if you notice any kind of rapid muscle gain or loss in body fat, your testosterone levels may be high.
Excessive Body or Facial Hair
Facial and body hair are often associated with masculine traits. But when they grow more densely or grow very fast, it is one of the solid signs of high testosterone levels. Many men notice thicker body and facial hair, like arm hair and beards, that grow very quickly (appearing seemingly overnight).
Oily Skin & Acne Breakouts
Excess testosterone can also overexcite oil glands, which leads to oily skin. Oily skin can clog pores, so acne is common. It often appears on the face, chest, or back. These stubborn breakouts are not occasional like normal acne, but quite persistent ones.
Shrinking Testicles & Fertility Changes
Another common high testosterone symptom in men is physical changes in the reproductive system. It may sound a bit strange, but one with high T levels experiences smaller testicles.
When the body senses too much testosterone, it suppresses its production, leading to testicular atrophy (shrunken testicles) and lower sperm count.
Enlarged Prostate or Urination Issues
Prostate health is closely tied to hormone balance. An enlarged prostate is another red flag. Too much testosterone can enlarge the prostate. It causes urinary issues like frequent urination, weak urine flow, or the constant urge to go.
Doctors note that men with very high testosterone may show signs like having low sperm counts and prostate enlargement.
Emotional & Behavioral Signs of High Testosterone in a Man
Excess testosterone affects the brain too, leading to visible changes in emotions and behavior.
Heightened Confidence & Aggression
Men with high T levels often feel sharper shifts in mood. One of the common signs includes sudden aggression or irritability. For example, you might get annoyed at small things or take more physical risks in sports or driving. This is because testosterone can heighten your risk-taking and competitive behavior.
Some of the medical sources list “aggressive or risk-taking behaviors” explicitly as a symptom of very high testosterone in men. You may also notice dramatic mood swings. One day you might feel on top of the world, the next day restless or anxious. This volatility itself is a high testosterone symptom.
Elevated Libido or Sexual Energy
High testosterone can also amplify your confidence and libido. It is a typical symptom of increasing testosterone. You may feel unusually bold, ambitious, or sociable. Your sex drive might hit an all-time high.
For instance, your interest in sex and frequency of sexual thoughts can increase markedly. A high sex drive is common with elevated testosterone.
Sleep Disturbances & Restlessness
Some men describe insomnia or disrupted sleep as a clue. They lie awake, racing with thoughts or energy.
Since testosterone can boost energy levels, it can also interfere with your sleep. If you are restless at night and keep turning and tossing all night, it might be due to high testosterone.
Other signs of high T in Men
Here are some other medically recognized signs of high testosterone in men that are worth paying attention to:
- Blood pressure changes
- Increased red blood cell production
- Unexplained headaches
- Swelling of legs or feet
- High cholesterol or liver strain
- Excessive sweating
- Changes in body odor
Can High Testosterone Cause Hair Loss?
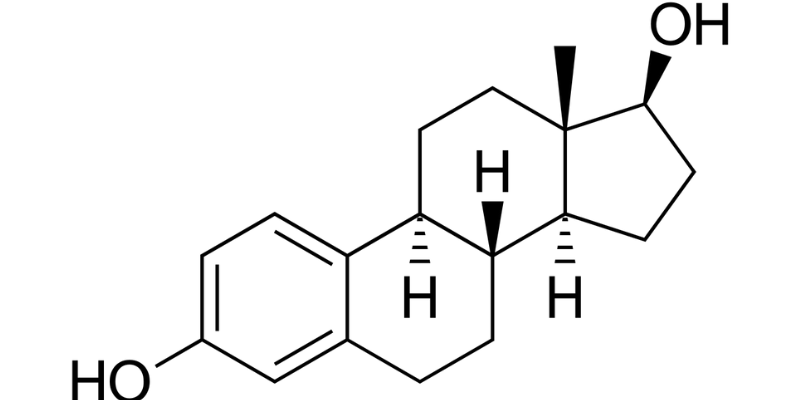
A very common question most men ask is, “ Can high testosterone cause hair loss?” The answer is both yes and no. Testosterone does not directly cause hair to fall out. It converts into another hormone called DHT (dihydrotestosterone).
Men who are genetically sensitive to DHT can experience male pattern baldness as the follicles shrink. Research notes that “high levels of DHT may have a higher chance of hair loss,” but this is not directly linked to testosterone levels.
That said, extremely high testosterone can shorten the growth phase of hair. If you think your hair loss is related to hormonal changes, you should get tested. But in general, hair loss is mostly affected by genetics rather than high testosterone.
What Causes High Testosterone in Men?
You can manage and prevent the symptoms of high testosterone by understanding the main cause.
- Anabolic steroids or testosterone supplements – These are used for bodybuilding or performance. These can increase testosterone far beyond normal levels.
- Hormone-producing tumors – Rare growths in the testes or adrenal glands may spark uncontrolled hormone release.
- Genetic factors – Some men, due to their genes, naturally run on the higher side of the T spectrum.
- Lifestyle changes – Major shifts in diet, training intensity, stress, and sleep can temporarily boost your testosterone levels.
- Prescription hormones (TRT) – These are used to treat the low levels of testosterone. But in some cases, they can also overshoot the ideal range if not carefully monitored.
- Endocrine disruptors – Certain chemicals in plastics and personal care items may throw off your hormone balance, up or down.
How to Treat High Testosterone in Men
The treatment of high testosterone depends on the cause. Some of you may need medical treatment, while others can normalize it with simple lifestyle changes. Here are the most common ways of treating it:
Stop or Adjust Testosterone Supplements
If you are taking any anabolic steroids or testosterone replacement therapy (TRT), you can consult your doctor to stop it or adjust the dosage. This is often the quickest way to lower your testosterone levels back into a healthy range.
Medication
Doctors may prescribe you medicines that block testosterone or lower DHT production. It is specifically if you are dealing with symptoms like acne, prostate enlargement, or hair loss caused by high levels of T. Some of the common medications include:
- Anti-androgens (e.g., spironolactone)
- GnRH analogs (for more severe cases)
- 5-alpha reductase inhibitors (to reduce DHT levels)
Treat the Root Cause
If the cause of your high testosterone is due to a tumor (in the adrenal gland or testicles), surgery or radiation may be required. Treating the root cause often restores the hormonal balance.
Lifestyle & Diet Adjustments
For mild cases, your doctor may recommend natural strategies to regulate your hormone levels:
- Reducing high-intensity workouts temporarily
- Cutting down on red meat, saturated fat, and sugar
- Avoiding over-supplementing with zinc or DHEA
- Managing stress through mindfulness or therapy
- Getting better sleep (at least 7 to 8 hours every night)
When to See a Doctor
If you observe any of the two or more of the following signs in your body, you should see a doctor.
- Rapid muscle growth or fat loss without changing your diet or training
- Persistent acne, oily skin, or aggressive breakouts
- Sudden mood swings, aggressive behavior, or sleep problems
- Testicular shrinkage, fertility concerns, or frequent nighttime urination
- Family history of prostate issues or sudden hair loss
Your doctor can run different tests and, depending on the results, will recommend the most effective treatment.
Bottom Line
Testosterone plays a very important role in a man’s body. And of course, more is not always good. High levels of testosterone in your body can lead to physical, emotional, and even reproductive changes. Some of them may feel like benefits to you in the beginning. But, they can quickly become uncomfortable and harmful if you ignore them.
If you suspect your hormone levels are off, don’t wait. At MD Longevity, we specialize in advanced hormone testing and personalized treatment plans to help you restore balance and feel your best.
Visit MD Longevity or call us at 888-545-3047 or 888-545-9147 to speak with a hormone health expert today.